Basic Life Support During COVID-19 Pandemic

Virus
Interview with Professor Peter Morley about basic life support for adults in the community during the Covid-19 pandemic.
Saving Lives Safely
Guidance on basic life support for adults in the community during the COVID-19 pandemicInterview with Prof. Peter Morley
Video courtesy of National COVID-19 Clinical Evidence Taskforce. Developed in partnership with the Infection Control Expert Group, Cardiac Arrest Working Group. Published: 22 October 2020 Note: Australia Wide First Aid training fully complies with Guidelines explained in this video.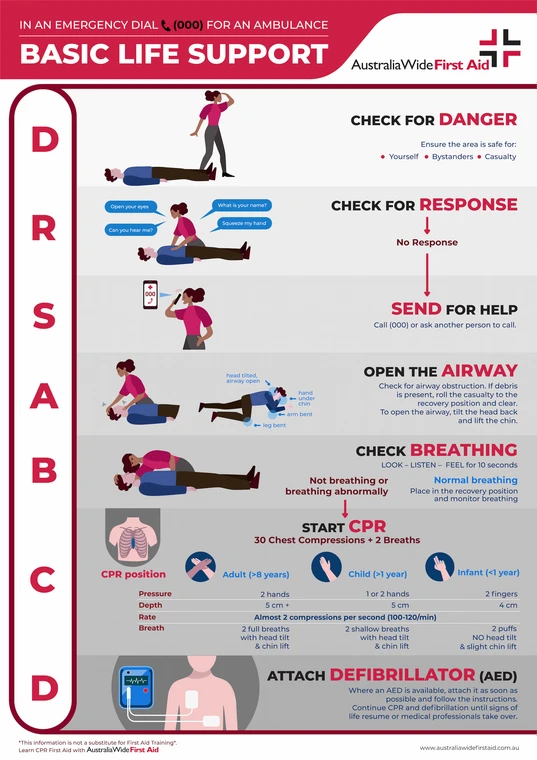
Guidelines for Basic Life Support During COVID-19 Pandemic
Video Transcript
Hi. My name is Peter Morley. I'm an intensive care specialist who works at the Royal Melbourne Hospital. I also have the privilege of chairing the Australian Resuscitation Council and the honour of being involved in the National COVID-19 Clinical Evidence Task Force. As part of that process, we set up a cardiac arrest working group and I had the pleasure of being involved in working our way through multiple iterations to get to this final outcome. The Taskforce developed the CPR flowcharts in partnership with the Infection Control Expert Group (ICEG). Who else was involved? There was a diverse group of people involved in that cardiac arrest working group — they were a combination of predominantly pre-hospital and emergency-based clinicians, but also, with a spread around Australia. The Taskforce normally makes guideline recommendations for use by clinicians in healthcare settings. Why did you decide to develop guidance on CPR in the community? We decided to start creating a chart for the community in particular, because there was a concern that the distress around Covid-19 might actually impact substantially on what goes on in the community. We know how important it is for the community to start basic life support and call for help early. And we knew that delays would result in worse outcomes for patients. Download the above flowchart as a PDF.The flowchart advises trained first responders to give chest compressions only (no breaths), if the person in cardiac arrest may have Covid-19. What are the other key differences for providing basic life support during the COVID-19 pandemic? The major difference is what we're recommending for situations where we think there may be a risk of COVID-19, is that we want people to consider that first line of danger to include thought around ‘what's the likely community transmission?’ And the consensus opinion is that if you're required to wear a mask as part of your local area, then the implication is you should treat the patient as if, potentially, they could have COVID. Now that means we want you to continue to wear that mask, covering your mouth and nose. But in addition, we want you to do a few other slightly different things. So, as the usual process is… if the patient is unresponsive, we want you to call for help. So please do that. But in addition to that, rather than getting close to the patient to see whether they're breathing or not, we just want you to look and see if they're breathing. If they're not breathing, start compressions… so, chest compressions in the middle of the chest. Hard and fast to their beat of Staying Alive. And then, as a defibrillator becomes available, use the defibrillator. Continue your resuscitation until expert help arrives and then, obviously at the end, we want you to consider washing your hands a little bit more explicitly than we would normally. We still think that this will double the chance of the person surviving to hospital discharge. So it's a really important thing. It's a very subtle modification to what we're doing and we'd like to think that this way will minimise the delays to resuscitation and improve the outcomes for all patients. Why is it so important to know how to ‘save lives safely’ during the COVID-19 pandemic? There is some published evidence throughout the world that there are some delays associated with the concern about COVID — and even evidence in Victoria suggesting some delays may have resulted in halving of the hospital survival rate for these people who have cardiac arrests out of hospital. So it is absolutely crucial that we do whatever we can to maintain the safety of everybody but also to minimise the delays to increase the chance of these people getting out of hospital alive.
Who is this flowchart intended for?
This sort of recommendation is relevant to all groups that are involved in providing basic life support, in other words, CPR to patients in the community. That might be late first aider organisations or people who are just trained health professionals providing who happen to be providing that sort of service. We don't usually recommend that this sort of recommendation would go to people who have never been trained in CPR but it is that sort of message which you can get across when you ring up the ambulance and ask for help. And the dispatchers can provide you with very simple instructions to allow you to do exactly what we're talking about. How significant is the risk of getting COVID-19 from providing basic life support? Now clearly the chance of someone having COVID is extraordinarily low in Australia. Even at the moment, it must be less than one-in-a-thousand. And so the chance of an individual getting an infection as a result of this process is extraordinarily low… especially if they're able to wear a mask and wash their hands appropriately afterwards. Most of the people that are actually unwell and possibly at risk of Covid have either been tested and isolated or are staying away from people. So we'd like to think that the chances are very, very low of anyone catching any diseases from people, with CPR. And that has certainly been our previous recommendations, even before COVID. What is the impact of giving chest compression only and not providing expired air resuscitation or ventilation (breaths)? With regard to the provision of expired air resuscitation or ventilation, we know that, from at least observational studies, people survive better if they do get a combination of chest compressions and ventilation. At some stage, ventilation is required for resuscitation of all patients. But, we believe, in the short-term, the risks and the benefits are probably in favour of not delaying starting because of a fear about doing ventilation. And the benefits of just doing chest compressions will still increase the likelihood of the person surviving. There is a high volume of COVID-19 research being conducted around the world. Do you expect more evidence to emerge that might impact these recommendations? The good thing about the living guidelines process is all the evidence that is being published — related to transmission of disease, or the impact of disease on the community — is being reviewed on a continuous basis. And these guidelines will be updated as required and are certainly going to be reviewed on a monthly basis at this stage. In Summary, who is this guidance intended for and how should it be applied? So these community guidelines apply to the resuscitations that occur in the community — but only up until the ambulance arrives. In this setting, the ambulance services around Australia have their own specific guidelines and the expectation is those specific guidelines would be adhered to in these situations. Overall, this is a really exciting process. I know that the COVID-19 pandemic has caused a number of concerns but the good thing is the Australian community works together to improve survival of people that have cardiac arrests out of hospital. And they're just simple messages that we can stick to, to double the chance of survival from a cardiac arrest.
Originally published at
https://www.australiawidefirstaid.com.au/resources/basic-life-support-during-covid-19
as part of the Australia Wide First Aid Articles Library